Prison Health: Finding Active Cases Early in the ‘World Behind the Walls’
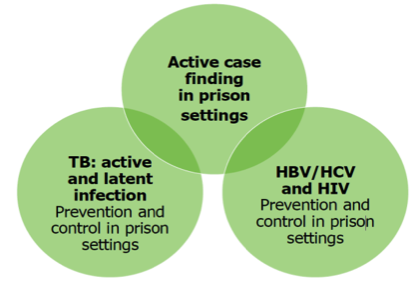
Communicable diseases, such as Tuberculosis (TB), Hepatitis C (HCV), Hepatitis B (HBV), human immunodeficiency virus (HIV), and Sexually Transmitted Infections (STI) like gonorrhea and chlamydia, are over-represented in prisoners.
A new guidance highlights that incarceration represents a unique opportunity to target groups that are usually hard to reach when in the community. The European Centre for Disease Prevention and Control (ECDC) and the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) recommend as a key measure the implementation of provider-initiated active case finding at prison intake.1 Early diagnosis, including testing for resistance, followed by an appropriate treatment initiation can prevent transmission of disease, both within prison and to the wider community. This contributes to public health prevention strategies.
|
|
For TB, a variety of different diagnostic tests are available for fast active case finding at prison entry. Their usage depends on various factors such as available resources, including laboratory facilities (at national & local levels) and national/international guidelines. Usually, risk-based or questionnaire-based, screening tools are not sufficiently sensitive and should therefore not be the only method. In contrast, sputum-based tests can be easily implemented because individuals can self-collect the specimens under supervision and deliver them to the healthcare staff. Rapid WHO-endorsed tests offer clear advantages, as they do not require an advanced laboratory, they provide rapid results and information on drug-resistance, and can speed up isolation and treatment initiation. Systems that enable co-testing for TB, HIV, HBV, HCV, and STIs from non-invasive samples provide an opportunity to meet the challenges of implementing an effective active case finding strategy in prison settings. |
References:
1. European Centre for Disease Prevention and Control, European Monitoring Centre for Drugs and Drug Addiction. Public health guidance on active case finding of communicable diseases in prison settings. Stockholm and Lisbon: ECDC and EMCDDA; 2018. https://ecdc.europa.eu/sites/portal/files/documents/Active-case-finding-communicable-diseases-in-prisons.pdf
New EU One Health Action Plan Against Antimicrobial Resistance
The European Commission (EC) adopted a new One Health action plan against antimicrobial resistance (AMR) in June 2017. There are three key objectives to the plan:
1. Make the EU a best practice region through better evidence, coordination, and surveillance
2. Boost research, development and innovation in order to control the spread of AMR
3. Shape the global agenda on AMR and the related risks
The EC recognizes that diagnostics are crucial for differentiating between bacterial and viral infections and identifying AMR, so that the most appropriate treatment can be given in a timely manner. Thus, the EC has stated that they will:
 |
|
The full report can be viewed here.
Reference: European Commission. A European One Health Action Plan against Antimicrobial Resistance (AMR). June 29, 2017.
New β-lactamase Inhibitor Combinations: Options for Treatment; Challenges for Testing
The differences in activity among new β-lactam/β-lactamase inhibitor combinations creates challenges for many clinicians and it will become increasingly important for microbiology laboratories to be able to produce meaningful results that will aid in the appropriate choice of these new agents. However, microbiology laboratories have few options available to determine the susceptibility of organisms to these novel antimicrobial agents as few of them are yet available on commercial AST platforms.1 Disk diffusion is the only option for testing some of these new drugs, but disks are often difficult to get. Clinical microbiology laboratories face a dilemma when it comes to providing information about the susceptibility or resistance of bacterial isolates to ceftazidime/avibactam and ceftolozane/tazobactam.
1. Humphries RM, Hindler JA. Emerging Resistance, New Antimicrobial Agents... but No Tests! The Challenge of Antimicrobial Susceptibility Testing in the Current US Regulatory Landscape. Clin Infect Dis. 2016 Jul 1;63(1):83-8.
Developing New Solutions – Cepheid’s GeneXpert System
Only when healthcare providers are able to identify whether an infection is present and if it is drug resistant in minutes rather than days, will we be able to move beyond empiric therapy. On-demand molecular diagnostics have the potential to do just that. Innovative new, on-demand diagnostics will help prevent the inappropriate use and overuse of antimicrobials and preserve our antibiotic weapons now and in the future.
If the world is serious about tackling the threat of drug-resistant infections, we need to fully embrace the step-change in technology that rapid point-of-care diagnostics represent.”
Rapid Diagnostics: Stopping Unnecessary Use of Antibiotics - The Review on Antimicrobial Resistance (2015)
Cepheid’s groundbreaking and innovative development pipeline aims to stay ahead of drug resistance and provide better stewardship solutions
Note:Slide the table to see more data
Available Now |
2017-2018* |
2019-2020* |
|
|
* Projected menu; subject to change.
O’Neill, J. Rapid Diagnostics: Stopping Unnecessary Use of Antibiotics - The Review on Antimicrobial Resistance. October, 2015.